From Cure to Comfort, the Role of Hospice Medical Director
 Dr. Robert Burns was approached by Crossroads Hospice as the company opened its Memphis facility in the late ‘90s, with the hope that he would become the site’s first medical director. Based on his work as an internist geriatrician at local nursing homes and the recommendation of an administrator, Crossroads was confident that he would be the best fit as the site grew.
Dr. Robert Burns was approached by Crossroads Hospice as the company opened its Memphis facility in the late ‘90s, with the hope that he would become the site’s first medical director. Based on his work as an internist geriatrician at local nursing homes and the recommendation of an administrator, Crossroads was confident that he would be the best fit as the site grew.
“Crossroads was starting out, so it was an opportunity to get involved with the company on the ground floor,” he recalls. “When I first started, our team meetings were to discuss only two, three, or four patients.”
The facility grew rapidly, as did the client base it served. With help from Dr. Burns, it was able to realize its mission of providing end-of-life care to a population that was, to that point, underserved.
“The way we started in Memphis was with a focus on the long-term care side and offering hospice care to residents of nursing homes, which at that time really wasn’t being done.”
The Team’s Medical Lead
As a medical director, Dr. Burns is responsible for two teams of patients, divided geographically. The patients’ case managers, responsible for the hands-on care, meet with him every other week to talk about issues and handle problems — clinical, social, or otherwise. Dr. Burns fields a variety of questions during these meetings and is available to address specific issues whenever they may arise.
Dr. Burns is in the office part of the morning for one day a week, then on-call the rest of the week to advise on medical solutions any time.
“The average day is attending a meeting, reviewing the patient cases that we’re discussing that day, problem solving for people who need it, and a variety of other things.”
Although making himself available remotely at all times can be a challenge, it is one he considers integral to his responsibilities as a Crossroads physician lead. The nature of this role means that Dr. Burns must trust his team, and they him.
“I can’t be with the patients all the time,” he says. “I rely on what is being told to me by my other team members. I trust in them, that they can assess and report to me what’s going on whether they’re nurses, social workers, or chaplains. We trust each other. We all bring different knowledge bases and skill sets to the team.”
Whether he is called for his input at noon or midnight, the unique chance to function and collaborate as part of a team is something Dr. Burns pinpoints as his job’s greatest reward.
“Everybody is equal and everyone has an opportunity to speak their mind.”
Success In The Face of Crisis
Dr. Burns considers a successful day of work one in which he has been able to alleviate a patient’s pain, whether that be spiritual, psychological, emotional, or physical. He works towards that goal in every case and finds success more often than failure.
“Given the challenges we face, with patient’s diseases, family dysfunction and life trauma, we are able to be successful more often than not. That’s important. When you get that person in pain finally at rest, when you get this family that’s dysfunctional to all get along, that’s rewarding.”
Some days, however, achieving complete comfort for patients is an insurmountable challenge.
“We can get people symptom free pretty quickly, but when you’ve got other issues to resolve as well, that’s a challenge. You feel frustrated because if they had been referred to us sooner or the family had been more responsive, you could have done more. That’s frustrating, when someone comes to hospice too late and we can’t do all of the things I think we’re capable of doing.”
Champion for Patients, Advocate for Hospice
As a physician, Dr. Burns sees firsthand the ways other healthcare professionals can misunderstand the role hospice should play for patients.
“We deal with misunderstandings from the medical community all the time,” he says. “The hospice industry is on the cutting edge of the spectrum of continuing care. We have a valuable service to offer people. The problem for physicians is that they are focused on curing people, making them better, and to change from that goal to comfort is something that does not necessarily compute.”
Outside of the office, in his interactions with the wider medical community, Dr. Burns is an advocate for the programs he knows to be crucial to patients and their families who are battling terminal disease.
“Hospice is a process. We can make you comfortable, but it’s more than that. It offers closure in patients’ lives. If you get handed off to hospice too late, there’s not a whole lot we can do towards that goal of closure. It’s frustrating, it’s very hard. It’s a barrier I’m trying to overcome, absolutely.”
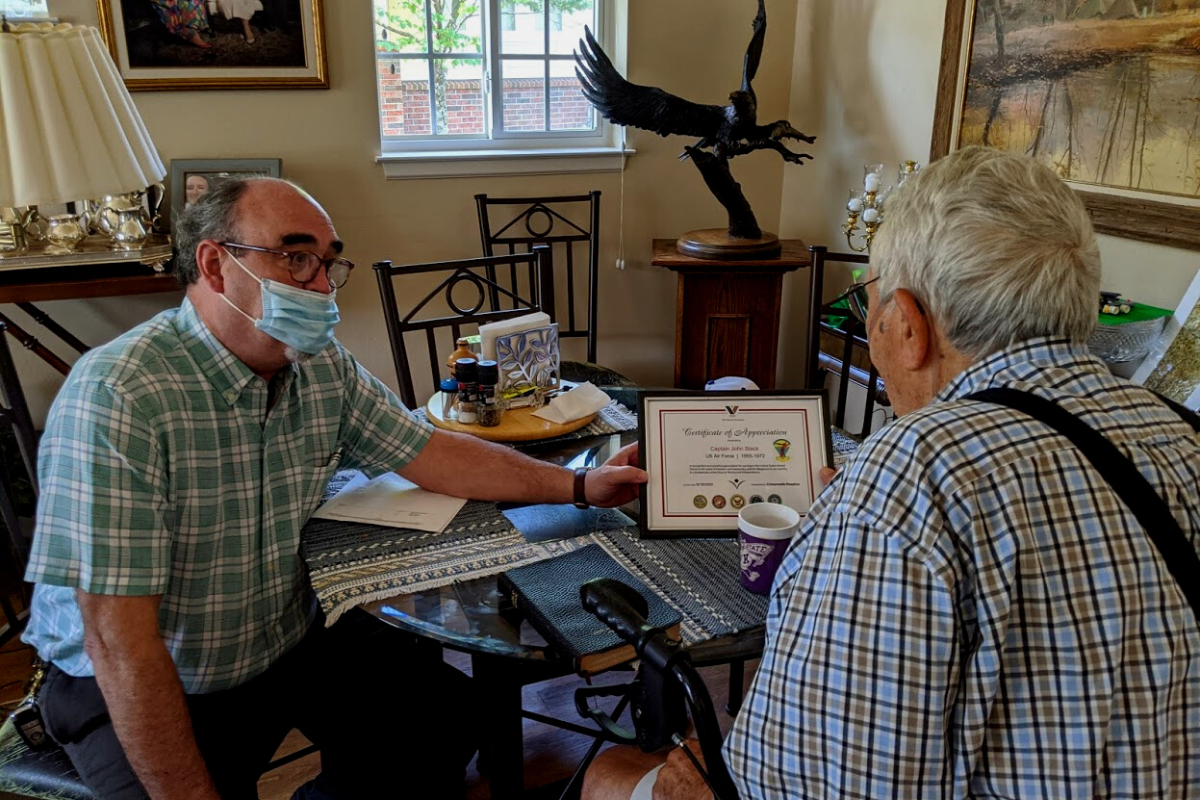
Honoring Our Medical Directors
We’re proud to honor Robert as our Crossroads Hospice “Staff Spotlight” recipient of the month, and recognize our medical directors who work tirelessly to serve our patients and families each day, such as Dr. Warren Stark in Lenexa.
If you found this information helpful, please share it with your network and community.
Copyright © 2015 Crossroads Hospice. All rights reserved.