Everyone Needs A Sense Of Hope
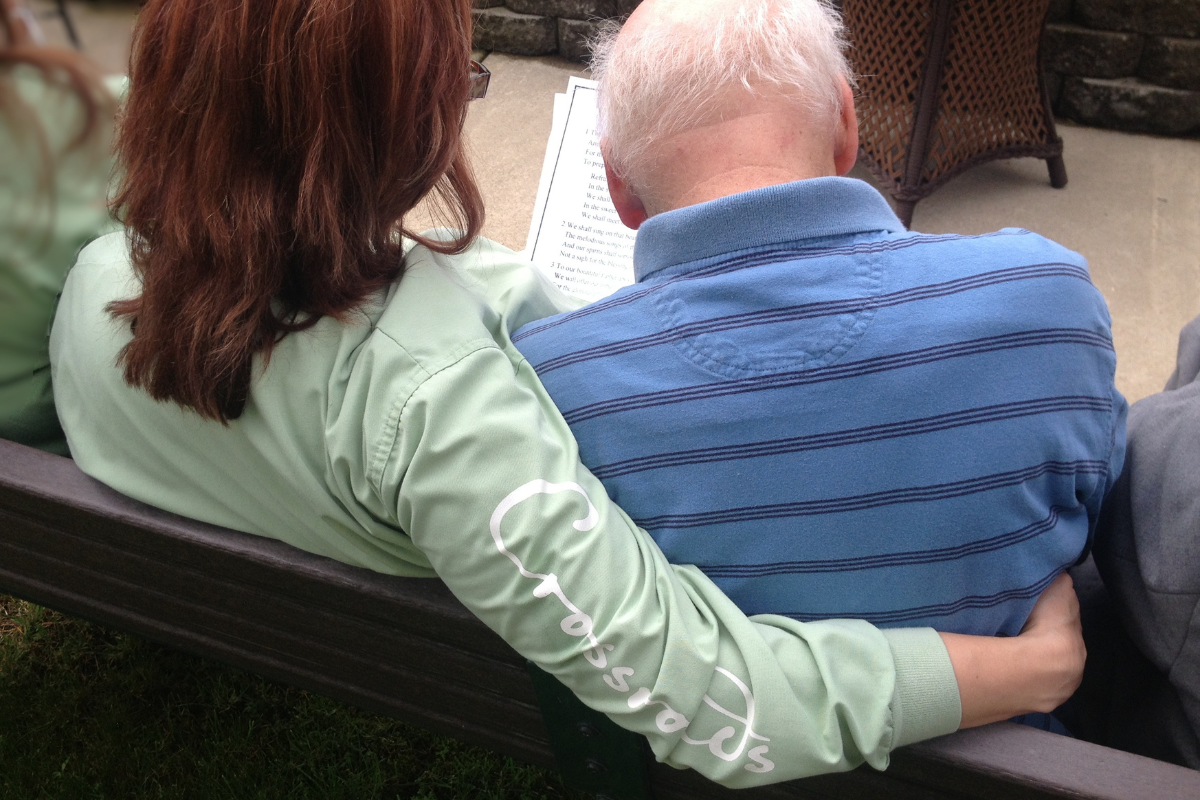
 When giving a diagnosis that a cure is not possible, that does not mean that the patient must be stripped of all hopes. In fact, it’s the exact opposite, because hope is vitally important in maintaining a happy and quality of life even during those hard times. This simply means that patients and families need assistance in focusing on realistically achievable goals and that is where Crossroads Hospice comes in.
When giving a diagnosis that a cure is not possible, that does not mean that the patient must be stripped of all hopes. In fact, it’s the exact opposite, because hope is vitally important in maintaining a happy and quality of life even during those hard times. This simply means that patients and families need assistance in focusing on realistically achievable goals and that is where Crossroads Hospice comes in.
Dr. David Casarett gives some insight on how physicians can give the support and hope their patients and families need when approaching end-of-life care.
It is recommended that physicians ascertain the patient and family’s understanding of the disease severity and prognosis. If there is a discrepancy between their understanding and yours, a conversation about patient goals (medical and otherwise) as well as patient hopes and fears can provide information that can lead to an empathetic delivery of bad news”.
For instance, a patient’s medical hopes might include at least a partial recovery, with non-medical hopes topped by a desire to see her granddaughter graduate from high school two months off. Fears might include concerns about pain and an intense dislike of the hospital. The physician could then initiate a shift-to-palliative-care discussion by beginning with a “wish statement”:
“I wish we could promise you a cure, but I’m afraid that is not likely. What we can do, however, is help you with your stamina so that you could enjoy your granddaughter’s graduation. That’s a very achievable goal. I also want to assure you that we can keep your pain at bay and that there are free services that can help you to remain at home if your desire is to stay out of the hospital…”
Certainly it will take time to emotionally process the shift from curative to a palliative-only approach, which is why it is advisable to have these discussions sooner rather than later. Professional opinion and several studies indicate that patients and families appear to receive optimal service benefit and express maximum satisfaction when they have received palliative care and the support ofhospice for 30-90 days before the death (Emanuel, von Guten and Ferris, 2000; Lynn, 2001; McCarthy, Burns, Ngo-Metzger, Davis and Phillips, 2003; Rickerson, Harold, Kapo, Caroll and Casarett, 2005; Teno and colleagues, 2004).
Through a focus on achievable goals, you can begin the move away from a curative focus while empowering the patient and family to define what hope and quality of life means to them.
Of course, some patient/families do not view a palliative-only approach as an appropriate treatment model. Particularly in the case of prolonged, chronic diseases such as congestive heart failure, COPD, and dementia, many patients and families do not grasp that these are ultimately fatal conditions. Dr. Casarett and colleagues (Casarett et al., 2005; Casarett, Van Ness, O’Leary and Fried, 2006; Casarett and Quill, 2007) suggest that an explanation of the progressive and fatal nature of the condition can help patients and families come to more realistic terms with their options. Mentioning to these patient/families that hospice may be a future possibility can plant a seed that can reduce resistance later should they come to accept the terminal nature of the condition.
For more info on how we can help you, help your patients click here.