New Year, New Health Choices to Consider: Palliative Care

It’s January, and families are facing some serious decisions about quality of life.
For some, it may mean a new gym membership. For others, it might mean looking for ways to ease the pain of a terminally ill family member through a regimen of palliative care.
This year, more physicians will be doing Advanced Care Planning. If you have Medicare, your doctor will be reimbursed for an appointment to discuss the type of life you want when ill.
What is palliative care?
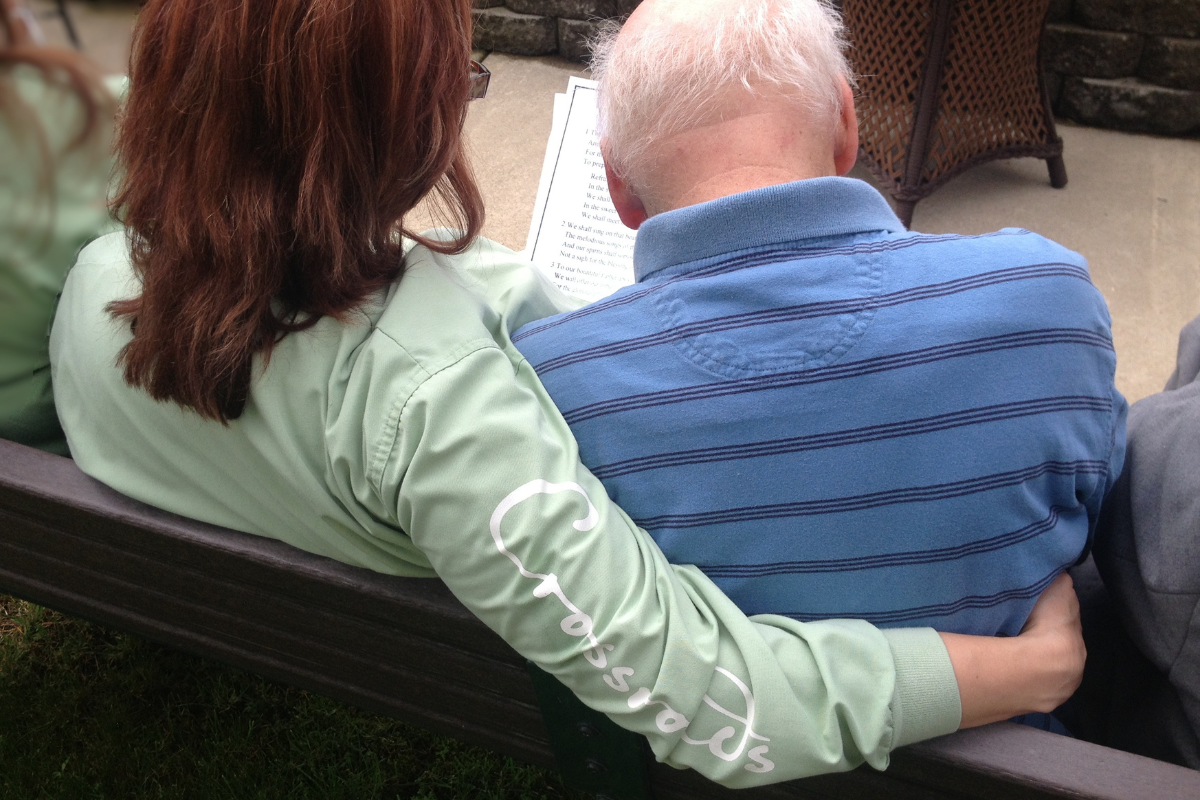
Palliative caremay be part of that conversation. This is medical care that aims to relieve patients from the symptoms, pain, and stresses of advanced illness—whatever the diagnosis. The goal is to improve quality of life and relieve suffering for both patient and family. Palliative care is appropriate at any age and at any stage in an advanced illness, and curative treatment doesn’t stop.
Palliative care is predicated on the patient making choices and knowing factors of his or her disease, and its symptoms, trajectory, and prognosis. During the conversation your physician explains the disease, different types of treatment available, their success rates and side effects, the impact on quality of life, and the various documents to consider to make sure your wishes are clearly stated. (These documents include advance directives, healthcare power of attorney, and Physician Orders for Life Sustaining Treatment, or POLST.)
Palliative care is about taking charge of your illness
“Palliative care is not about giving up,” says board certified palliative care physician Dr. Tim Ihrig, medical director for palliative care at Trinity Regional Medical Center in Iowa. “In fact, studies with cancer patients show that those who receive true palliative care have less depression, undergo less chemotherapy, spend less time in the hospital, have a higher quality of life, and eventually, are more likely to die at home on hospice. In addition, they live longer than without true palliative care.”
“Palliative care puts the patient in the center of the healthcare hub, encouraging the patient to call the shots on the goals of care and intensity of care-exemplifying true informed consent,” says Dr. Ihrig.
Most of us prefer to be in the driver’s seat when dealing with a serious disease like cancer, COPD, cardiac disease, ALS, or HIV/AIDs.
The patient as educator
We all need to educate ourselves on palliative care. Not all physicians are familiar with it. Certainly not all doctors focus their attention on palliative care or have a board certification in the specialty. You may need to search to find the right doctor with whom to have that talk mentioned earlier.
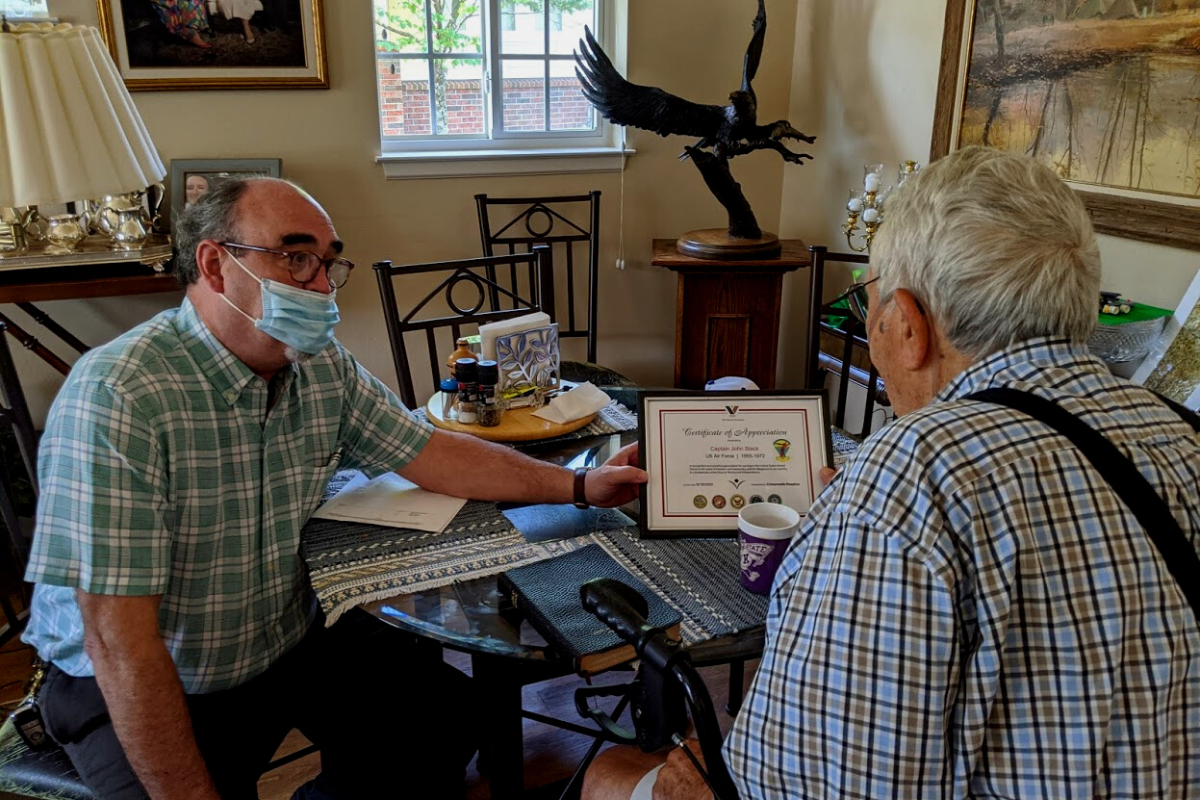
Finding a palliative care team
Some hospices have palliative care programs. Make sure that the one you contact has board certified palliative care physicians and staff, and that the program is distinct from hospice, as Crossroads Palliative Care is. Not all hospices work this way.
You can learn more by searching “hospice vs. palliative care” online. (Our own Dr. Walter George has a great video that explains the difference.) Or, check out Dr. Ihrig’s TED Talk. He’s a national expert on the topic and Crossroads' Chief Medical Officer.
If you found this information helpful, please share it with your network and community.
Copyright © 2016 Crossroads Hospice. All rights reserved.