Palliative Care for Veterans with Serious Illness

When Veterans are faced with a chronic or advancing illness, memories from years of combat may revisit them throughout their care. These thoughts can be linked to emotional, spiritual, or psychosocial traumas and can place additional strains on their quality of life and their loved ones.
“We don’t know what they’ve seen. We don’t know what they’ve been through,” says Lindsay Nobel, a nurse practitioner at Crossroads Hospice & Palliative Care in St. Louis.
Because of these unknown factors, it’s important to be aware of what to expect when those moments arise and how to take advantage of the programs and resources available to them.

Learning to talk about pain.
At the core of palliative care is a higher level of communication that aims to ensure patients and their caregivers understand all aspects of the issues at hand. Many Veterans don’t open up about their time on the battlefield, whether it’s because of shame, humility, or frustration. So helping them communicate in a productive way is a key component to managing their overall health – even when that involves anger or tears.
“A lot of that is acknowledging the difficulties that they have been through and allowing them to express those,” says Nobel. “Sometimes they’ve never been given that opportunity to open up and be emotional without being judged.”
These conversations begin with asking open-ended questions and not making assumptions. This may be challenging at first, especially if a Veteran has shut down previous conversations. But providing them with the empowerment to share their feelings can lay the groundwork for an honest conversation to unfold. When patients are able to voice the pain they are holding onto, the less likely they will have pent up emotions that can lead to restlessness, agitation, or anxiety – all common side effects of post-traumatic stress disorder (PTSD).
When Veteran patients struggle with open communication, Crossroads’ Vet-to-Vet program is available to connect them with Veteran volunteers who have been recruited because of their similar backgrounds. Oftentimes, Veterans empathize more easily with someone who has walked in their shoes. Together they can bond over their shared sense of brotherhood and speak freely about their past experiences.
“There is a lot of emotional and physical pain that laymen who haven’t been in the military don’t know about, so it helps them to be able to have that outlet to speak to,” says Nobel.

See the signs and know their meanings.
Many patients with a chronic or advancing illness will encounter some form of depression and various stages of grief as a result of their condition. This may lead to them isolating themselves from friends and family. For Veterans, this can manifest on a much larger scale.
It’s important to be aware of any big or sudden changes to a patient’s mental health and behavior. If they are typically socially active and excited to spend time with others, but start to withdrawal, family members and caregivers should check in with them and allow them to vent. Later, they should reevaluate their care needs with their physician so that their palliative care team can address the issues.
It’s also important to understand that potentially traumatic events endured while being at war may mimic similar feelings and sensations in a patient’s body and mind. For instance, Veterans who were starved or water boarded during combat, says Nobel, might experience the same type of anxiety when they are not hungry from taking medication. Talking to the patient about how this chapter in their life is not punishment can help alleviate some of their distress.
Every visit with a palliative care team will be different for patients as they utilize different resources available such as social workers and volunteers who can help lend an open ear through these challenging times – especially when the circumstances feel like they are rapidly evolving.

Recognize their service and document their life.
Not all Veterans want public recognition. Many believe it was simply “their duty” to serve. But for those who do want to commemorate their achievements, learning about their life and showing appreciation during this difficult time can make all the difference in the world.
Crossroads is a proud partner of the We Honor Veterans program – a collaboration between the U.S. Veterans Administration and the National Hospice and Palliative Care Association. This program is made up of hospice and palliative care organizations across the nation with a goal to increase Veterans’ awareness of these services and continually improve the quality of care.
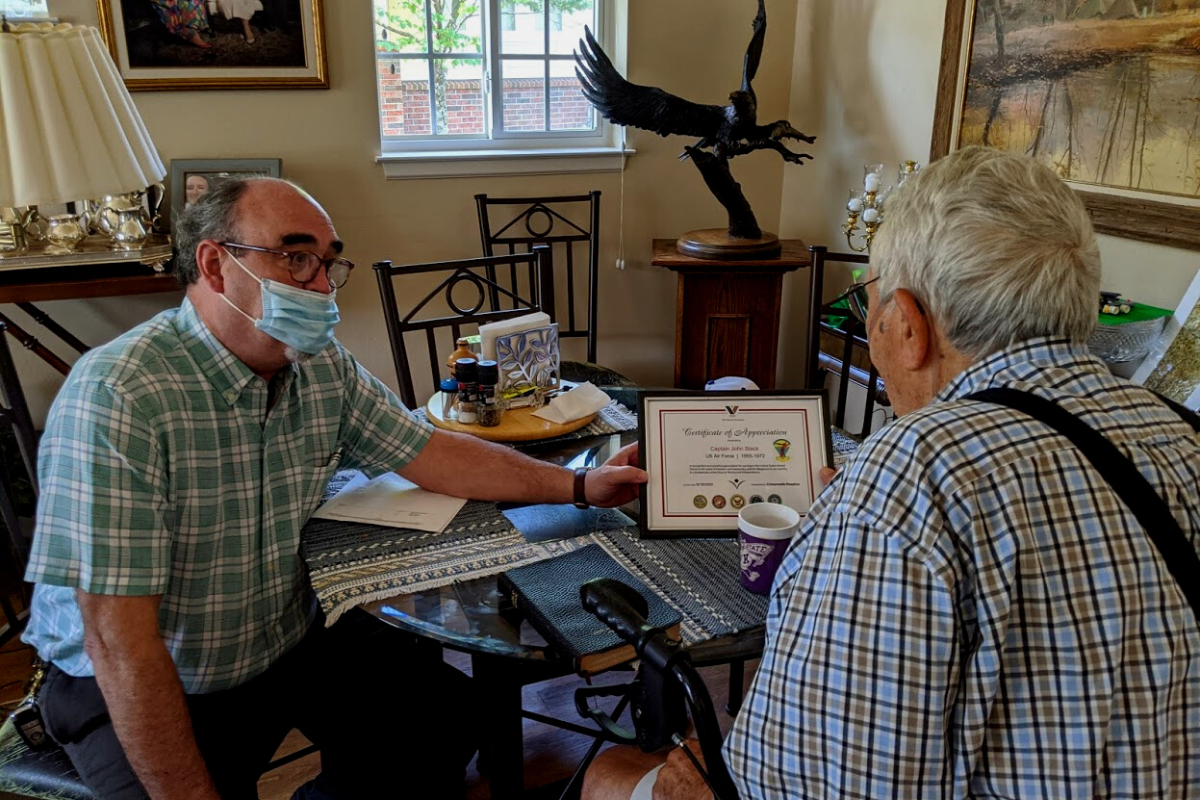
At Crossroads, a cornerstone of a Veteran’s plan of care, should they want it, is a Veteran Recognition Ceremony that pays tribute to both Veteran patients and their family members for all that they have sacrificed for their country. During this ceremony, patients receive tokens of gratitude that include a certificate of appreciation that recognizes their service. More importantly, they receive the presence of their loved ones, volunteers, and palliative care team to remind them how special they are. Crossroads recognizes over 3,000 Veterans each year.
Beyond these programs, there are other great ways to honor Veterans throughout their battles with chronic, advancing illnesses. One option would be to help them tell their story through joining the Veteran History Project. This program preserves the stories of American war Veterans for future generations. Another option to show support for Veterans would be to make a donation to an organization like the Wounded Warrior Project, which is committed to helping Veterans overcome some of these unique challenges they face.
For more information on how Crossroads supports Veterans, visit our website or call us at 1-888-564-3405.
If you found this information helpful, please share it with your network and community.
Copyright © 2019 Crossroads Hospice & Palliative Care. All rights reserved.